5 Miscarriages, 5 IVF Cycles and Balanced Translocation: Columbia’s Infertility Journey
“It’s easier to talk about my infertility journey than not. People don’t want to bring it up but it’s already up. It’s everywhere I go and everywhere I look. It’s constant.”
“I always had a feeling I would struggle with infertility, but there was never any reason for that except just fear. When we decided to start trying, we ‘pulled the goalie’, if you will, and while I didn’t necessarily expect it to happen quickly, I hoped it would. When we started trying to get pregnant, we were relaxed and positive. But when we still weren’t pregnant at the eight-month mark, I went to my doctor who told me I was young and healthy, didn’t need a test anything, and casually told us to stay out of the hot tub at the end of the visit. She said the hot tub could affect male fertility, which was interesting because my husband had built a hot tub in the backyard, and we were in it almost every night. I read that it takes 60-90 days for sperm to regenerate and 64 days after my husband put the hot tub away, we were pregnant for the first time. On December 03, 2018, I got my first positive pregnancy test.”
Unfortunately, Columbia’s path to motherhood wouldn’t be that easy or that fast. At the first ultrasound, the baby was measuring behind and the tech suggested that maybe Columbia had the dates wrong. She had convinced herself that maybe the tech had the measurements incorrect, and everything was fine when obviously they were not. Waiting to go in for her second ultrasound, she started to miscarry at home on January 4, 2019. She had spent Christmas and New Year’s pregnant, so excited only to have it end quickly. This first pregnancy marked the start of what would be an incredibly hard journey filled with much loss and heartache.
WHEN ONE MISCARRIAGE QUICKLY BECOMES TWO
“We took a little break after our first loss and when we started trying again, I was pushing hard for different tests to be done and asking lots of questions. I was getting a lot of ‘I don’t know’ responses and realized I had been seeing midwives and not even a doctor. So, I switched to an obstetrician (OB) and that same month we got pregnant for our second time. The day we learned we were pregnant again, there was a massive rainbow in the sky and while I’ve never been very religious, I saw that rainbow and thought ‘okay, this is God’. The test line wasn’t dark, but I was so sure this pregnancy would stick.
My OB brought me in for a blood draw to see where my human chorionic gonadotropin (HCG) levels were, and it wasn’t increasing very much between the first and second test and then we got the call saying my HCG was actually going down. I asked what that meant, and the nurse said it meant it wasn’t a viable pregnancy. Again, I asked what that meant and if there was anything else I could do only to find out there was nothing we could do. We were having another miscarriage. The next day I started miscarrying on my birthday when I turned 32. My birthday was kind of ruined for a while after that.”
DISCOVERING BALANCED TRANSLOCATION
“After the second loss, my OB decided to do a full panel of recurrent loss testing and because I was going to the OB instead of a fertility clinic, I was able to get it covered by insurance. They drew about 11 tubes of blood and I remember thinking that this was serious. As I was waiting for results, I was researching as much as I could and decided that my biggest fear would be if I ended up having a blood clotting issue, because then I would have to do injections…Joke’s on me!
When the blood clotting test came back normal, I assumed everything was normal and our two miscarriages were just bad luck. We also learned that my anti-müllerian hormone (AMH) was 0.699, which didn’t concern my OB and we were waiting on one more test. On October 28, my husband proposed to me and on October 29, I got the call from the OB, diagnosing me with balanced translocation. I had no idea what it meant.
The balanced translocation really meant that we were at an increased risk of miscarriage and again, I asked what exactly that meant. The OB informed me that some people with balanced translocation do IVF but that it wasn’t always necessary. I had a conversation with my husband after learning all this and basically asked if he was sure he wanted to marry me because I had no idea if I was going to be able to give him a family. His answer: ‘you’re my family.’ Brownie points for him saying the right thing!
When we met with the genetic counselor, they told me my risk of loss per pregnancy was around 30%, which was low given the circumstances. The interesting thing about balanced translocation is that everyone’s odds are different, and everyone’s translocation is different. I’m also not sure if anyone else in my family has balanced translocation but if you don’t have insurance, getting a karyotype test to find out if you have translocation can be about $1000 USD.”
WHEN A POSITIVE TEST FEELS LIKE A POSITIVE MISCARRIAGE
“I was at the point where a positive pregnancy test was not a baby…the positive test meant a miscarriage. It was just a question of when it would happen, not if.”
“We decided to take a break from trying to conceive and focused on getting married and planning a wedding. During this time, I had also decided not to go back on birth control. My cycles were pretty regular, and we decided we would just be careful with our timing. At one point we had sex and I expected to ovulate about 10 days later, but it ended up being five days early, but I wasn’t worried about it because it had taken me a long time to get pregnant previously and I wasn’t buying into the idea that sperm could live for up to five days. Well, there was a way, and Thanksgiving 2019 I took a pregnancy test and the test was positive. I looked at the test and thought it had to be a joke.
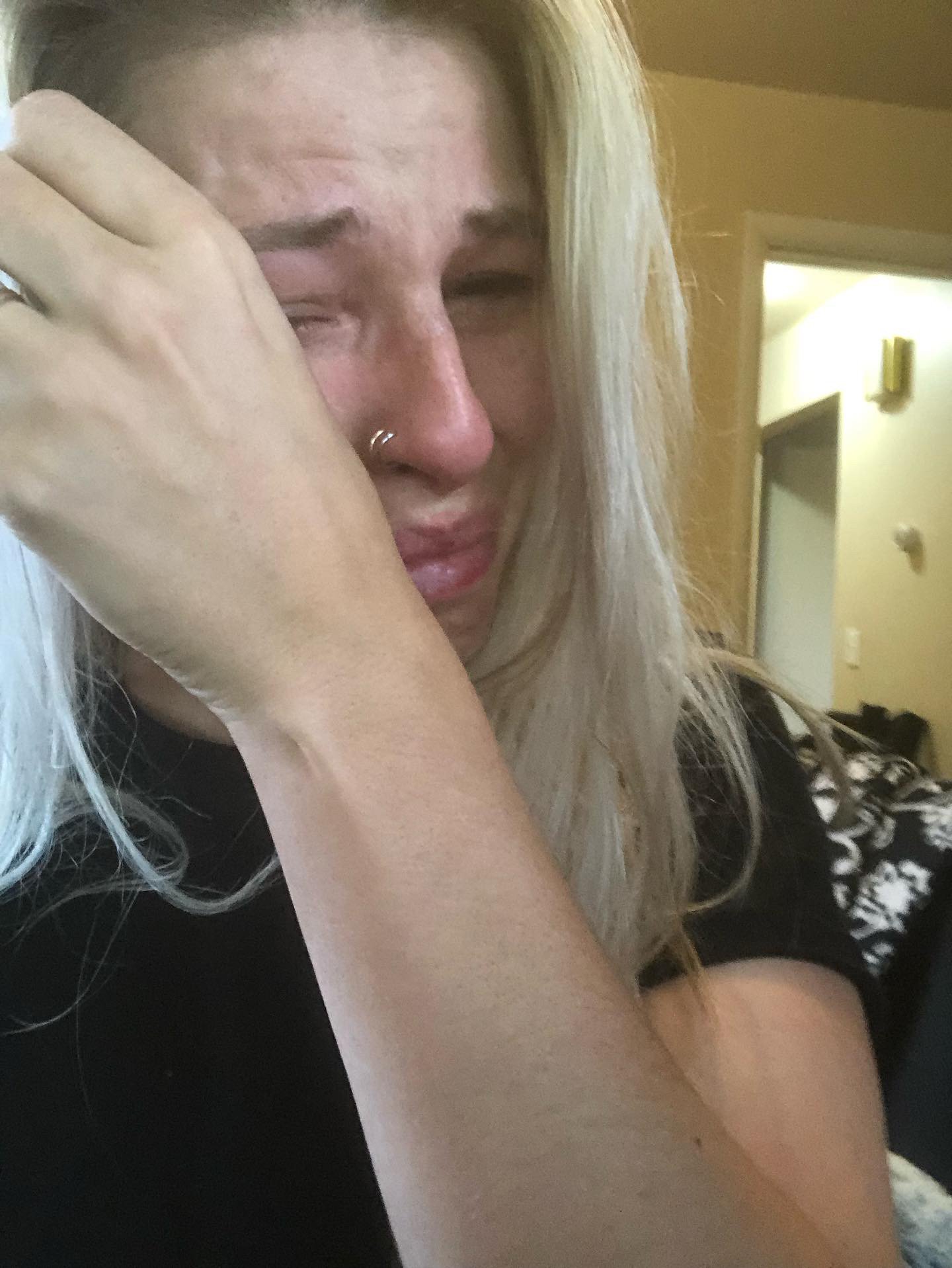
I went up to my husband to share and he said I had ‘that tone’! I shared that the test was positive, and I just started crying because I didn’t want to miscarry again. My last miscarriage was the beginning of October and here it was November, and I just wasn’t ready to miscarry again so soon. I was at the point where a positive pregnancy test was not a baby…the positive test meant a miscarriage. It was just a question of when it would happen, not if.
When you have recurrent pregnancy loss, each miscarriage hurts differently. For the first miscarriage, you’re shocked because you never thought it would happen to you. After the second miscarriage, you think it will never happen again because everyone talks about how your body will know what to do now that it’s been pregnant once already. During the third pregnancy, you try to find a way not to get your hopes up, so it doesn’t hurt as much but of course it does. No matter what, each miscarriage crushes you in a new way.”
THIRD PREGNANCY…THIRD LOSS
“I was so sure I would miscarry with the third pregnancy, but I still calculated out my due date. We had planned our wedding for August 01, 2020, and we would be due on August 07, 2020. Realizing that, we put wedding planning on pause but didn’t cancel anything because I had no idea how it would turn out. At the beginning, my betas were going up almost perfectly and two days before Christmas we went for our first ultrasound and everything was perfect there, as well. When I was two weeks, three days the doctor saw a small subchorionic hemorrhage but thought everything looked great otherwise.
What is subchorionic hemorrhage? A subchorionic hemorrhage is when there is bleeding beneath the chorion membranes, which enclose the embryo in the uterus. The bleeding is thought to start when there is a partial detachment of the chorion membranes from the wall of the uterus.
We had a trip to Mexico planned at the end of January 2021 and I insisted that we do another ultrasound before leaving the country. I explained how I was so scared we would miscarry while in Mexico and the office came up with a plan to have me come in and see a nurse to have a doppler done. I would be 10 weeks and three days at that point, and they thought we would be able to find the heartbeat.
“I always say hope is relentless…the thing that keeps me sane is my community of infertility sisters and feeling supported by other people who have been through their own infertility journey.”
My husband couldn’t get out of work and so I brought my best friend with me to the appointment. The nurse looked around and couldn’t find the heartbeat and I thought it was just because they were using the doppler and I was only 10 weeks along. So, they got me in for a quick ultrasound and I stared at the screen thinking I was going to see our baby. I knew what the heartbeat should look like, and I could see right away that there was no heartbeat there.
They confirmed there was no heartbeat, and I was beside myself, bawling. Even more upsetting was seeing my best friend completely heartbroken and devastated for me. It was horrible. They said I could have a dilation and curettage (D&C) procedure that evening, and I just wanted to get it done. Through testing, we learned it was a boy, but we never did get an answer about what might have caused the loss because they didn’t find any genetic issues.”
TIME TO MEET WITH AN REPRODUCTIVE EMBRYOLOGIST
“We got married in August 2020 and immediately started trying again. We got pregnant in October 2020, but it was a chemical pregnancy and we loss the baby super early.
We then decided to try medicated cycles, thinking that if we could get multiple follicles, we might have a better chance of getting a good follicle to fight against the translocation, and get pregnant faster. I was ready to get this show on the road. We did a total of five medicated cycles, none of them worked, and we decided we were done with that.
At this point, I wanted to see a fertility specialist to see if they had any other testing they would recommend. I still wasn’t convinced we would do IVF, but I felt like my OB was running out of ideas. My OB referred me to Seattle Reproductive Medicine in Spokane, WA and I started with a virtual appointment. The doctor was 10 minutes late to the Zoom call, spent 10 minutes explaining straightforward COVID protocols, and cut me off while I was working through the questions I prepared, which we didn’t even get through. I was so frustrated because that consultation was $300 USD for me to sit in front of a Zoom call for 40 minutes and not have any of my questions answered.
The only real takeaway from the consultation was that she wanted to test my antral follicle count (AFC) and she thought my AMH looked low. At that point, we were encouraged to really look at IVF as an option and the most pivotal thing the RE said was that if I didn’t do IVF, I would not have more than one child. I took it to heart despite knowing some of her other points were wrong, like saying with my balanced translocation I’d miscarry between 10 and 12 weeks. I didn’t have a lot of faith in her and felt like she was patronizing. She was more interested in being heard rather than hearing what I had to say or ask.”
A NEW REPRODUCTIVE EMBRYOLOGIST…BUT FIRST, ANOTHER MISCARRIAGE
“I decided to do my own research and found another fertility clinic in town. Because I shared that I was thinking about switching clinics, they gave me the consultation for free and we were able to meet in person. I went to the consultation in May 2021 with a new perspective that we were going to move forward with IVF.
The new RE had a picture of my chromosomes sitting on the table, which I’d never seen before, and he had a thick file with all my information he had gathered. He knew so much about me before I even sat down, and it felt like such a great sign. He did not rush a single second and I even shared with him that I heard his bedside manner wasn’t the best, but I didn’t need to like him and just needed him to do a good job. He thought we could do both.
I felt confident and wanted to keep moving forward with the new RE. He offered to do an ultrasound that same day to see where we were at, and we went from his office straight to the ultrasound room. We had been trying and I knew I was seven days post ovulation and my boobs hurt. I kept thinking ‘just watch me be pregnant right now’, and sure enough I was pregnant.
My betas were doubling perfectly, and I thought maybe we would be the anecdote where we were just about to start IVF and a miracle happened! When we went in for the first ultrasound, the baby was measuring behind and I knew, nope, this pregnancy wasn’t going to happen. It was done. The ultrasound tech was very sweet and tried to convince me otherwise and I told her that I knew my body, I knew my diagnosis, and I also knew this was going to be a miscarriage.
“There are so many ways it can go wrong and even though so much of this process is out of my hands, I still feel responsible for them.”
The miscarriage was a blighted ovum and dragged out, stuck in a limbo of being pregnant and not pregnant. We had approval to do the D&C and after testing, we learned it was a girl with normal chromosomes. I questioned why we were even doing IVF if the point was to do IVF to get normal embryos. This last miscarriage showed that I had normal embryos but was miscarrying them. The new RE was blunt with me and said that he thought if I didn’t go forward with IVF, I’d always wonder what would happen if I had.”
WHEN IVF IS MET WITH DISAPPOINTMENT
“We qualified for the embryo banking program at my clinic, which is usually reserved for women over 40 years old. Lucky me! We qualified because our situation was so bad. The program was a $30K USD fee and the clinic would cover four retrievals and one transfer. The $30K USD was the clinic fee and didn’t cover any medications, anesthesia, or embryo testing but it was still a bargain. I wanted to bank as many normal embryos as possible because time was against me, and I had translocation. This felt like my best chance and for the best deal.
All my rounds of IVF have been disappointing. We got five eggs in my first round, and I was devastated because I had seen other people getting 20+ eggs. All five of the eggs were mature and fertilized, we got two embryos, and then both were abnormal. One round done and nothing to show for it.
We started our second round of IVF, and it was even worse. We didn’t change anything about my protocol and decided to cancel 10 days in because I only had two follicles. After cancelling a cycle, I started to push for more changes in my protocol and the RE decided to increase my dose of Follistim for round three. We got nine eggs and five were mature, and four fertilized. However, we still unfortunately got zero embryos from round three, with nothing to show.
I had another consultation with my RE after round three and asked him to look at everything to see what else we could do. I asked if we could add Clomid given how I responded during my medicated cycles; We didn’t get pregnant, but I had lots of follicles and my progesterone was sky high. The RE genuinely looked curious at my suggestion and decided to add Letrozole to my last cycle. It was my best cycle in terms of the numbers but still not the overall results we were hoping for. I got 14 eggs, 13 of them were mature and fertilized, and only two embryos. Obviously, that was a huge letdown and right now, I have an email in my inbox asking me to pay $800 USD to test my embryos and I’m hoping and praying that by some miracle, we have some normal embryos.”
SCARED TO GET A NORMAL EMBRYO
“I’ve said out loud before that I am afraid to get a normal embryo. I’m afraid because that means that I’m in this position where I have a mile long list of things that I want to check off to try and make my body the safest place I possibly can for the embryo. I should see a naturopath, I should do acupuncture, I should go see a reproductive immunologist, I should do the hysteroscopy, and the list goes on. There are so many ways it can go wrong and even though so much of this process is out of my hands, I still feel responsible for them.
“The doctors tell you that miscarriages are so common, but if it’s so common, why don’t they know how to deal with it?”
Everyone loves to say that it only takes one…one egg or one embryo. But I’ve already lost two and twice my body has shown me that it can’t carry a ‘normal’ baby because we know that neither had balanced translocation. And I can’t help but think what if the transfer doesn’t work? Plenty of people have failed transfers and for no known reason. I know that I can get pregnant because of my history, but that doesn’t mean that an embryo transfer from IVF will get me pregnant and keep me pregnant.”
HOPE BOMBS NOT NEEDED
“One of my friends the other day talked about how people like to ‘hope bomb’ you and tell you not to lose your faith. But who said I was losing the faith? Do you see me stabbing myself with needles every day, all in attempt to have the baby we so desire? I have all the faith.
I’ve always been very open about my infertility journey, and I’ve seen a massive shift over time with how people react to me and how people treat me. It started with things like ‘oh, don’t worry about it, just relax’, or ‘it’ll happen next time’ to ‘I know somebody who had so much worse than you and now they have two kids.’ Now, people generally don’t say anything to me and completely avoid the topic. You can see that they are so uncomfortable, and they have realized that I shut down the clichés.”
FINDING SUPPORT IN FAMILY AND FRIENDS CAN BE HARD
“My relationships with my family and friends have changed since going through infertility. My mom has been through rigorous training by me about what to say and what not to say to someone on this infertility journey. It’s been mostly by trial and error that she has learned, and specifically by error. After my loss, she’s commented on how at least I didn’t have a baby with birth defects and that it wasn’t a real baby but just a ball of cells. She’s also talked about how hard the journey has been on her and how she doesn’t know how to treat me because she doesn’t want to upset me. I love my mother and with time and experience, she has gotten so much better.
It can also be hard with friends. One of my dear friends is pregnant and she found out she was pregnant on the first day of my first round of IVF. It was really hard. She’s about 20 weeks pregnant now and I’m realizing I’m going to go through five rounds of IVF while she goes through this one pregnancy. It’s crazy to look at that kind of timeline comparison.
The thing that keeps me sane is my community of infertility sisters and feeling supported by other people who have been through their own infertility journey. Those women get it and can commiserate with me and listen to me. They don’t feel like they need to lift me up, fix anything, or try to make anything better.”
I’M NOT THE SAME PERSON I WAS BEFORE INFERTILITY
“The emotional burden? I shouldn’t laugh, but I’m not the same person that I was before starting this infertility journey. In the past four years since we started this journey, what matters to me has changed. And I don’t just mean becoming a mother. It’s how I interact with people and how I want to do something that truly matters for the world. I now advocate for myself and feel strongly about advocating for others. But the emotional toll has been very heavy.
There is a never-ending heaviness going through infertility and I can look at a photo of myself from five years ago and see a different look in my eye. I’ve been crushed as a person in so many ways. And it’s not just pregnancy loss…it’s a loss of a future. It’s a never-ending fear not knowing what’s on the other side and not knowing if I will ever be a mother. That’s a hard thing for people to grasp if they think infertility is just about not being able to get pregnant. Being infertile impacts your whole life.
“There is never-ending heaviness going through infertility and I can look at a photo of myself from five years ago and see a different look in my eye.”
Yesterday I had a cup of tea, and I was looking out the window in my kitchen toward the backyard and I was just thinking about the future my husband and I have dreamed about together and what it looks like without kids. We plan to move out of the city sometime soon and thinking about our future, I was picturing this big house with a beautiful backyard and imagining how painfully quiet our house will be. Without kids our house is full of emptiness. My back seat is empty. When going through infertility, you look at the rest of your life with that possibility of emptiness and there isn’t a way to fully explain that feeling to someone who hasn’t ever thought about or had to face that possibility. I’m faced with it every single time bad news comes our way on this journey.”
FEELING LIKE DOCTORS DON’T CARE
“The most shocking part of my infertility journey has been how much doctors don’t care. They don’t care about your fertility. What they care about is keeping you from getting pregnant and then taking care of you after you do get pregnant. There is no coverage for anything else in between those two things.
How doctor’s offices handle miscarriages is where I see the most opportunity for change. The doctors tell you that miscarriages are so common, but if it’s so common, why don’t they know how to deal with it? The ultrasound techs who do your initial evaluation aren’t trained in how to interact with you or tell you that your baby has no heartbeat. Women calling from the front desk don’t know what to say when they’re trying to get you scheduled for your next appointment but you’re trying to tell them your baby died. It’s what has frustrated me the most.
Every office should have a list of counselors that are available and have experience specifically with miscarriage loss. They should schedule follow-ups to see if you’re dealing with postpartum depression. They should have procedures in place that automatically turn off all appointment reminders after you miscarry. I’ve gotten reminders throughout an entire pregnancy in the patient portal reminding me to schedule my birthing class.
I actually think it’s important not to trust your doctor, in the sense that you should take everything at face value. Keep asking questions and a good doctor will be open to those questions and should have answers. You want a doctor who will not be frustrated by you doing your own research and asking questions but will be curious and open.”
FOR THOSE WALKING THE PATH OF INFERTILITY
“It’s okay to be mad, sad, negative, upset, and jealous. It’s okay to feel your feelings. Just be careful what you act on because there is no reason to pretend this is a journey filled with light and positivity.
There is a lot of hope. And I always say that hope is relentless. It comes back even when you are in your darkest moment, and that is how we continue to keep fighting this fight.
But don’t think you have to sugarcoat the journey for anyone else’s comfort because you don’t.
I get tired of people accusing me of being negative when I’m just trying to protect myself. I must be aware of all the possibilities and a lot of them are negative. It is possible I won’t get any embryos and it is possible I will walk away from this entire journey without a child. And if people dismiss me when I say that, they’re just doing it for their own comfort. It has nothing to do with me.”
Since talking with Columbia, her story and her family have grown. You can continue to follow Columbia’s journey and see how she continues to uplift and support others battling infertility on Instagram @yearning.into.motherhood.