A Cystic Fibrosis Diagnosis, Two Losses, and Three Transfers to Get Pregnant: Allison’s Infertility Journey
“My grief and pain will never go away, and I’ll always wonder what could have been with our lost babies. But I can say that it does get a little easier with time.”
Allison knew a lot about the human body in general, about human anatomy, physiology, her cycle, etc. and she knew battling infertility was always a possibility, but she never thought it was going to be a part of her story. Allison is a goal-oriented person and when she decides to do something, she plans, prepares, and achieves it. Right after she got married, her husband and her knew they wanted to start trying to have a baby right away and they had it planned out just like every other big decision. Allison was going to get off the pill on a particular month, they were going to get married, and then they knew what month they would start trying. Of course, it did not go according to that plan at all and instead they walked the path of infertility that was filled with one curveball after another.
SIX MONTHS OF TRYING AND WE’RE STILL NOT PREGNANT
“I went off the pill in May 2019, we got married in July 2019, and while we didn’t start off tracking anything, we were hopeful that we would get pregnant right away. I’m not a patient person and by September we weren’t pregnant, I started to track my cycle more closely with ovulation tests and our timing. In December, I reached out to my OBGYN and shared that after six months of trying, I had this feeling that something was wrong because I was ovulating, we were timing everything perfectly, and we weren’t getting pregnant.
We did routine blood work to check my thyroid, estrogen, and FSH and it was uneventful. The only thing my doctor saw was that I had borderline polycystic ovarian syndrome (PCOS) but I was still ovulating most of the time and while my cycles were a little irregular, she didn’t see it as a huge deal. My doctor thought my body needed a little help to ovulate better and put me on Letrozole. We tried that for five cycles, and I ovulated every time, timed it great, but no pregnancy.”
MALE FACTOR INFERTILITY: THERE IS NO SPERM IN THE SAMPLE!
“It was around March 2020 that my doctor decided we should test my husband. She didn’t expect to find anything and told me it was very rare to have male factor infertility. I vividly remember the weekend we found out the results from his semen analysis. My husband called me first and shared that there was no sperm! I was so confused and when the doctor called me directly and she said there was zero sperm in the semen sample, and she recommended we see a urologist for further testing.
At this point, we knew nothing at all and our whole world instantly shattered. It was terrible and a low point of our journey that felt so long because we had to wait a couple of months to see the general urologist in June 2020. He did bloodwork on my husband, did an ultrasound of his testicles, and again, everything was normal and looked great. His recommendation was to put my husband on six months of Clomid, which in males can help create sperm and increase estrogen.
We were naïve and so hopeful at this point, thinking that this could be our fix. I think I was a bit more skeptical than my husband and immediately started researching other things that could be factors we weren’t considering. My research showed men with normal blood work and zero sperm typically have an obstruction of some sort because when it’s non-obstructive, the follicle stimulating hormone (FSH) levels are high, which my husband did not show. I felt like something else had to be going on.
It was a long six months of my husband taking Clomid and us waiting, grieving, and hoping that this was going to be our solution. The urologist retested my husband’s sperm sample in December 2020 and again, it was zero. The general urologist was out of ideas and didn’t know what else to do. He actually said a comment to my husband that we’d find out if the Clomid really worked if he could get me pregnant. I knew at that point we were done, and it was time to find a new specialist who could help us.”
“My husband called me first and shared that there was no sperm…At this point, we knew nothing at all and our whole world instantly shattered.”
MY HUSBAND HAS OBSTRUCTIVE AZOOSPERMIA
“We had a friend of friend struggling with severe male factor infertility and they recommended a fertility urologist at OHSU. I reached out on my own and it was the best decision we ever made. We got on the cancellation list and got lucky when we grabbed a spot to see the new fertility urologist in January 2021. We drove to Portland and not only was the doctor amazing, but he was also optimistic. He thought there was an obstruction going on but couldn’t be positive without further testing. He did a physical exam, another ultrasound, and more detailed bloodwork. He also included a cystic fibrosis gene sequencing panel and that was the winner! My husband was diagnosed with obstructive azoospermia due to cystic fibrosis (CF).
My husband does have a lifelong history, especially as a child, with hay fever, seasonal allergies, bronchitis, and things like that but no one ever thought it was something to consider. Finding out he had cystic fibrosis was a shock and we learned that van deferens in males with CF, or a variant of CF, does not form appropriately. The sperm is there, but without the van deferens, the sperm cannot get out.
They completed a full gene sequencing to see which genes my husband carries, and we learned he carries one of the classical CF gene copies and then one non-classical CF gene copy. That’s the reason he doesn’t have classical CF symptoms but technically still has a CF diagnosis. It’s what they call nonclassical CF.”
IVF IS THE ONLY WAY WE CAN GET PREGNANT
“Getting the call about my husband having CF was honestly good news for us because it was the first time in over a year and a half that we had a clear-cut answer and some true hope. We also had a clear direction forward, and we knew that they only way we could conceive was through IVF, with a sperm retrieval, and intracytoplasmic sperm injection (ICSI). Thankfully, OHSU had a great reproductive endocrinology team that was on the same floor as our fertility urologist. He put in a referral for us, and I was able to get started with the IVF process.
While I got started with IVF, they did a testicular biopsy on my husband to ensure there was sperm. They froze his sample and thawed his sample to make sure it would survive the thaw for IVF and at the end of March 2021 we received the best phone call saying there was plenty of sperm! They froze four little straws from the biopsy and thought it was subjectively enough for four rounds of IVF.
Before getting started with our first round of IVF, it was also recommended that I also get tested to see if I was a CF carrier, although they said it would be rare for both of us to be carriers and we likely had nothing to worry about. Coincidentally, my dad had gifted me the 23andMe and Ancestry kits and it had just been sitting around the house. I went ahead and sent in my results and those results came back a week before the clinic’s results and I could see that I was also a CF carrier. I carry one normal copy and then I have the classical copies that cause classical CF. We were told that our combination of CF was very rare and made us the 1% of the 1%, and after everything we had been through, I wasn’t the least bit surprised.”
“I was naïve and thought we would be one of those couples who would have a successful retrieval and be pregnant after a single transfer.”
FIRST CONSULTATION AT THE IVF CLINIC
“My first consultation with the IVF clinic was in June 2021 after I continued to call asking if they had a cancellation. They did all the initial bloodwork and ultrasounds and there was nothing to lead them to believe that I would have any issues with the IVF process. The biggest issue we had was creating embryos and they were optimistic that once we got through that step, I would have no issues getting pregnant. I was naïve and thought we would be one of those couples that would have a successful retrieval and be pregnant after a single transfer.
It wasn’t until August that we started my meds for my first cycle and because I had borderline PCOS, they thought I would be a high responder. Therefore, they put me on a lower dose of medication but for whatever reason, my body did not respond to the medication. I kept going in every couple of days for routine checks and on day nine, they were expecting me to have over 20 follicles and there were only four.
We had to weigh our options and decide if we would waste a retrieval, knowing that we were probably going to lose a lot of embryos after testing the embryos for CF, or if we would cancel the retrieval and start over. We decided to cancel the retrieval on Day 10 and that was incredibly disappointing because we were so optimistic that this was going to work.
The waiting continued from September to November. I let my body come off the meds and ovulate, releasing the eggs I did have, which was a little painful and then we had to start over with another retrieval. But those two months felt like forever, especially because we can’t try naturally. There’s never that little hope that maybe we’ll have a miracle before we start the next round of IVF because with my husband’s diagnosis, that’s never an option for us.”
CREATING OUR FIRST VIABLE EMBRYOS
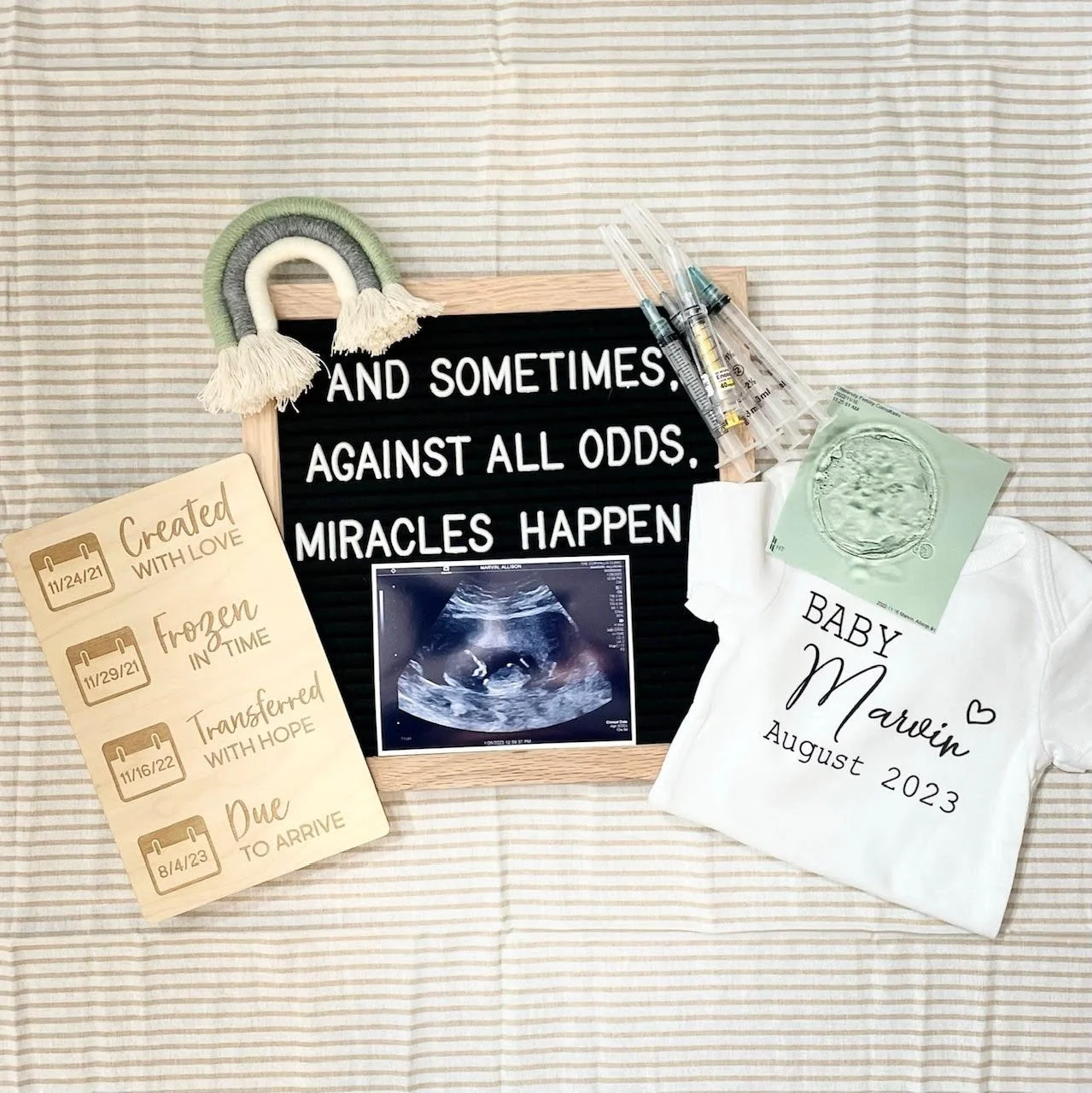
“In November 2021, we tried another round of IVF with a higher dose of meds, and I had a much better response. We ended up retrieving 24 eggs and out of those 24, 13 were mature. Nine of those eggs fertilized with my husband’s sperm using ICSI and eight of those made it to the blastocyst stage. We sent those off for genetic testing, which took about eight weeks. They had to set up what they called a probe to test for the CF and took samples from me, my husband, and cheek swab samples from our parents, as well. This allowed them to map out the specific gene mutations that we have, to then test our embryos for those mutations.
We decided to only do preimplantation genetic diagnosis (PGT-M) testing for CF and didn’t do preimplantation genetic screening (PGT-A) testing for chromosomal aneuploidy because the clinic thought I was young and probably didn’t have to worry about it. Out of our eight embryos tested, one had classical CF and the others were a random mixture of both my husband and my gene combinations.”
“Losing our baby girl at nine weeks was horrible…I would lay in bed literally just screaming and crying thinking that there was no way that I was ever going to get over this.”
TWO TRANSFERS AND TWO LOSSES
“In January 2022 we were ready for our first transfer, so excited, hopeful, and convinced that it was going to work the first time. Unfortunately, we had an early chemical pregnancy loss, and it was incredibly hard, especially because it was the first time my body had even had the chance to be pregnant.
When we went back to the clinic in February, we found out I had a couple of small polyps that had likely grown from the high estrogen I was taking during the stimulation. I had to have a hysteroscopy to clean the polyps out and by May 2022 we were ready for our second transfer. We transferred two embryos and found out that one stuck and we were pregnant. However, at the six- and seven-week ultrasounds, our baby girl was measuring small and seemed to be growing slowly. We went in for check-ups three weeks in a row and I was just waiting for them to give us the bad news and at our nine-week appointment, her heart had stopped, and we lost her. They called it a missed miscarriage because my body didn’t recognize it.
Losing our baby girl at nine weeks was horrible, and the lowest point in our journey for sure. I tried to avoid the D&C and opted to take the medication at home. Thankfully mom came over and was with me for a couple of days because the process was traumatic. It was super painful, with cramping and bleeding and then the actual passing of it was so difficult emotionally and physically.
At this point, I wanted to take a break and insisted that we do further testing because I now had gotten pregnant twice but lost both pregnancies. We did a full recurrent pregnancy loss (RPL) panel and made the decision to have our four remaining, non-CF embryos PGT-A tested. Everything on the RPL testing was normal except for one blood clotting marker that was slightly elevated. So, they added Lovenox, steroids, and baby aspirin to my next transfer.”
“I was terrified of being pregnant and having another miscarriage, but I was also terrified of never being pregnant again.”
TERRIFIED TO TRANSFER ANOTHER EMBRYO
“Out of the four embryos tested, three were normal and one had Klinefelter syndrome (a genetic condition where a male has an extra X chromosome), which we wouldn’t transfer. We elected not to find out the genders of the three remaining embryos to keep one thing a surprise and it wasn’t until November 2022 that we did our last transfer. This transfer felt different than the first two. We were excited to be trying again but I was terrified this time around. I was terrified of being pregnant and having another miscarriage, but I was also terrified of never being pregnant again. I went into the transfer anticipating the roller coaster that was to come.
I took it day by day for this last round and especially for the first nine weeks, as I was very much waiting for the other shoe to drop. But it never happened, and everything has been great for this pregnancy. The baby has been growing great, the heartbeat has been great, and I’ve felt great.”
BLEEDING AT 15 WEEKS WITH PLACENTA PREVIA
“We waited to announce this pregnancy until after the first trimester. It was around 14 weeks when we graduated from our clinic and announced to friends and family. Right after that at 15 weeks, I had a huge bleed out of nowhere. My first thought was ‘here we go again’.
A trip to the emergency room and they determined that I had an anterior placenta, and the baby was thankfully ok. It took a few weeks to figure out that my placenta was very low over the cervix, and it was a placenta previa. When the placenta migrated and moved up, it caused a big hemorrhage, which caused the bleed. After two big bleeds and spotting for a few days, I stayed on bedrest and thankfully it cleared up, the placenta slowly moved away from my cervix, and I haven’t had any issues since.”
“There is so much trauma attached with going through infertility…There are moments when you must allow yourself to say you don’t want to do any of this.”
EMOTIONAL BURDEN OF INFERTILITY
“The physical part of IVF was not a big deal. The needles didn’t bother me, and it was just something that I had to do. I took the mentality that this was the hand we were dealt, and IVF is the only way that we’re going to grow our family biologically.
The emotional part of infertility was what was so hard. The unknown is consuming: Not knowing what the outcome was going to be, not knowing if anything we were doing was going to work, not knowing if we would have to do another cycle.
There is also so much trauma attached with going through infertility and PTSD. You are always being dealt bad news and through it all you continue to try to stay positive for your partner and yourself, but there are times when you admit that this sucks. There are moments when you must allow yourself to say you don’t want to do any of this.
Even now that I’m pregnant and closer to birth than not, it’s almost a surreal feeling thinking how I have really gone through all of this. When I first shared my journey with my therapist, she told me that she counted 10 major traumatic life events in the past three years. When you hear your story back and hear someone reflect what you have gone through in that way, it truly hits how hard it is to go through this journey.”
“No one goes into starting a family thinking it’s going to take two losses and three transfers to get pregnant, and that’s after you go through IVF…the unknowns of infertility are the hardest part of this journey.”
HOW TO KEEP MOVING FROWARD DURING INFERTILITY
“Sometimes I don’t know how I kept going on this journey of infertility. I remember being so angry and so sad at certain points. I would lay in bed, literally just screaming and crying thinking that there was no way that I was ever going to get over this. But I knew that I had to and so we took it one day at a time.
My husband’s grief was different than mine, but he was still able to support me and let me process however I needed to process in that moment. Some days were relatively okay and some days I was not okay, and I stayed in bed all day. But what it took was waking up every day, putting one foot in front of the other, and breathing.
My grief and pain will never go away, and I’ll always wonder what could have been with our lost babies. But I can say that it does get a little easier with time.”
FINDING SUPPORT THROUGH INFERTILITY
“I found support through my friends, my husband, and my mom. When I created my Instagram account, that also helped tremendously, because going through infertility can feel very isolating, especially with a unique diagnosis like ours. It was hard to find people who were in a similar situation and being able to connect with people through the online community helped me talk to people who truly understood what we were going through. Those conversations gave me the confidence to share our own story and help others realize that what we are going through is more common than anyone ever realizes.”
“I can’t tell others to stay positive because there were many days where I was not positive. But when you are going through the trenches and you are taking it day by day, keep breathing.”
INFERTILITY IS FULL OF CURVEBALLS
“One of the most shocking parts of infertility for me has been all the potential curveballs that nobody ever thinks can or will happen. No one goes into starting a family thinking it’s going to take two losses and three transfers to get pregnant, and that’s after you go through IVF. No one thinks they are going to be a carrier for these genetic mutations that can prevent you from getting or staying pregnant. But the unknowns of infertility are the hardest part of this journey.”
FOR THOSE WALKING THE PATH OF INFERTILITY
“I want to encourage others to keep breathing and to keep going.
I can’t tell others to stay positive because there were many days where I was not positive. But when you are going through the trenches and you are taking it day by day, keep breathing.
Going through infertility is not easy and I do not wish it upon my worst enemy. It was hell to go through but also know you are stronger than you think you are. That is one thing I have realized as we have gone through hell and back to get to this point and my husband and I are closer now because of it.
Keep fighting. Keep going.”
Since talking with Allison, her family has grown, welcoming their little girl into the world. You can continue to follow Allison’s journey and see how she continues to uplift and support others battling infertility on Instagram @mrs.allisonmarvin_ivf.